Mental health harms have become synonymous with people who use methamphetamines. However, individual study results are often inconsistent. This this has made it difficult to draw firm conclusions about the risks.
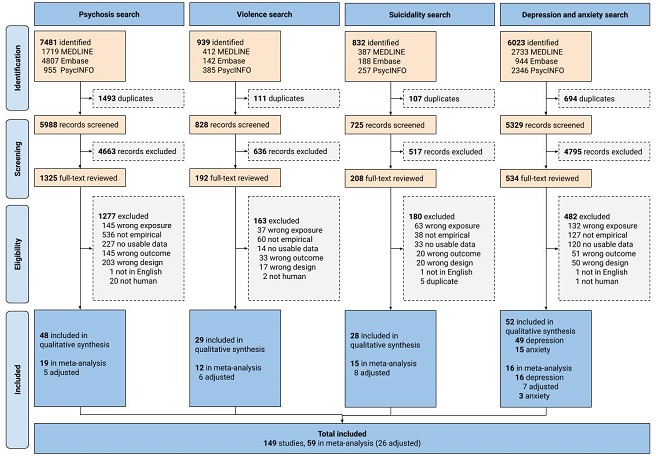
We conducted the first global systematic review and meta-analysis of over 15,000 scientific articles and 149 studies on the association between the use of amphetamines and each of these mental health outcomes: psychosis, violence, suicidality, depression and anxiety.
The findings confirm that people who use methamphetamine are at a significantly elevated risk of poor mental health when compared to people who do not use the drug. We found that they around twice as likely to experience depression and psychosis and four times more likely to be suicidal. The review also revealed other significant findings.
- Services that interact with people who use methamphetamine need to have the capacity to treat and manage co-occurring mental health conditions.
Currently services for substance use and mental health are often separate, meaning that people who use substances do not get the care they need for mental health issues.
More work is needed to ensure that people who use this drug are provided with adequate mental health care. We need to tailor generic responses make sure they are acceptable, safe and effective for people who use methamphetamine.
- The elevated risk of psychosis is a major concern
There is currently no agreed treatment model for people who have methamphetamine-related psychosis. These people are often released without a care plan for their psychosis, resulting in a “revolving door” scenario.
Psychosis is often dismissed as being “drug-induced” but the reality is that many of these people will experience recurrent psychotic episodes (often triggered by ongoing methamphetamine use) and some will go on to develop schizophrenia. Treatments that can stop this progression need to be developed and put in place.
- Depression and suicidality, while less dramatic, are often more common
These are important issues in their own right, but they also make it hard for people to break the cycle of using methamphetamine. The high from using methamphetamine relieves depression, but when people stop using (i.e., go through withdrawal) the depression gets worse. This can lead to a downward spiral.
Some antidepressants can interact with methamphetamine and this can increase the risk of side-effects. We need to know more about what antidepressants work for people who use methamphetamine. We also need to apply strategies that we know work more generally to reduce suicide risk, even screening and brief intervention. Psychological therapies can also reduce the risk of depression and suicidality, and these need to be implemented.
There is an urgent need to develop epidemiological research on the use of amphetamines and mental health outcomes in order to better quantify and mitigate this risk. In the meantime, clinical responses to the use of amphetamines need to become better integrated and resourced to enable the management of these co-occurring conditions.
Citation
McKetin, R., Leung, J., Stockings, E., Huo, Y., Foulds, J., Lappin, J., Cumming, C., Craig; A., Arunogiri, S., Young, J., Sara, G., Farrell, M., & Degenhardt, L. (2019). Mental health outcomes associated with the use of amphetamines: A systematic review and meta-analysis. EClinicalMedicine. Advance online publication. doi:10.1016/j.eclinm.2019.09.014
About the author
Associate Professor Rebecca McKetin (BSc(Psychol)Hons. PhD) leads a program of research into stimulant use epidemiology and interventions at the National Drug and Alcohol Research Centre, UNSW. Her current research involves the online delivery of psychological help for people who use stimulants, the trialling of new pharmacotherapy options for methamphetamine dependence, and the development of novel responses to methamphetamine use in Aboriginal and Torres Strait Islander communities.
Rebecca established the first longitudinal treatment outcomes study for methamphetamine use internationally (the Methamphetamine Treatment Outcomes Study, MATES), a 3-year prospective cohort of 501 people dependent on methamphetamine, demonstrating the impact of community-based treatments for this drug. She has adapted in-direct prevalence estimation methods to estimate the number of dependent methamphetamine users in Australia and has been involved in the development of regional systems to monitor methamphetamine and other drugs in the Asia Pacific.
Rebecca’s work has been pivotal in quantifying the risk of psychosis, violence and other mental health outcomes related to the use of methamphetamine. She is a Senior Editor for Addiction, a consultant to the United Nations, and a member of the Australian Institute of Policy and Science.


