There were 15,743 hospitalisations with a drug-related principal diagnosis in Victoria in 2020-21, equivalent to 0.54% of all hospitalisations in Victoria.
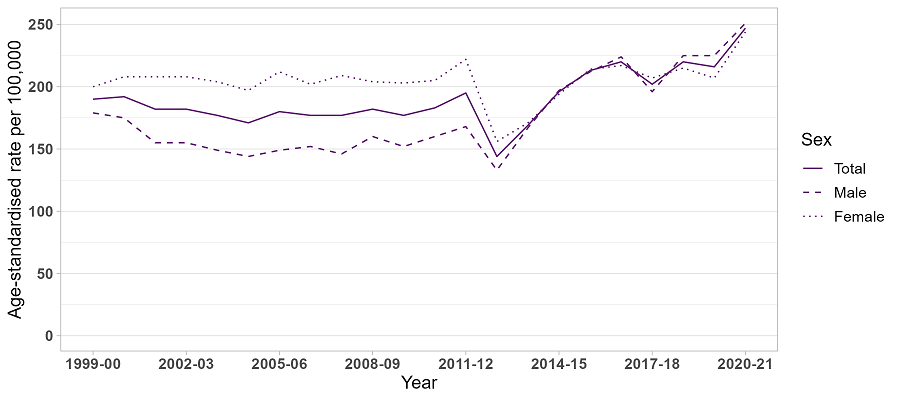
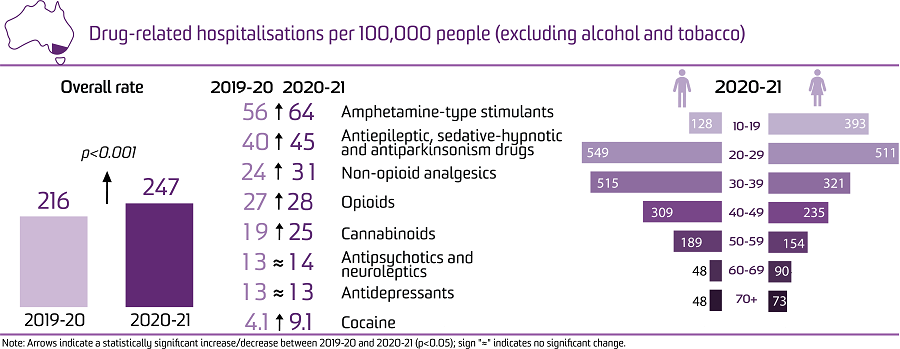
This is equivalent to 247 hospitalisations per 100,000 people, which was a significant increase from 2019-20 (216 hospitalisations per 100,000 people; p<0.001), and the highest rate over the course of monitoring.
Sex
The rate of hospitalisations was higher among males than females in 2020-21 (251 versus 244 hospitalisations per 100,000 people, respectively).
Age
In 2020-21, the rate of hospitalisations was highest among the 20-29 age group, followed by the 30-39 and 40-49 age groups (532, 417, and 272 hospitalisations per 100,000 people, respectively). Among both males and females, the rates of drug-related hospitalisations were highest in the 20-29 age groups.
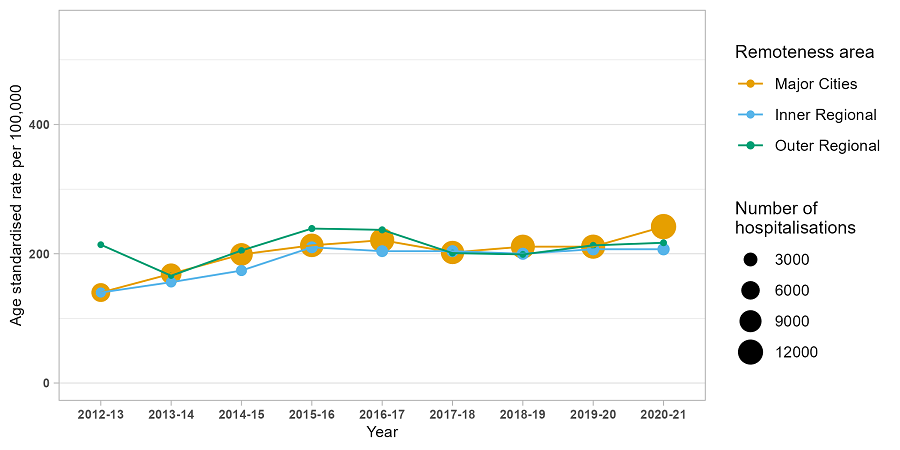
Remoteness Area of Usual Residence
The highest number and rate of hospitalisations in 2020-21 was observed in major city areas (12,279 hospitalisations, 242 hospitalisations per 100,000 people).
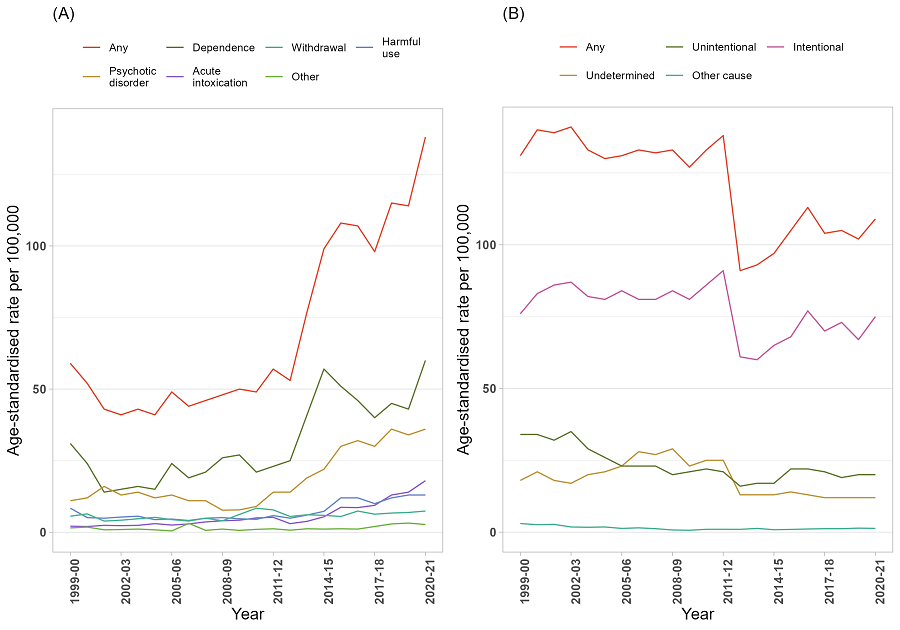
External Cause of Drug Poisoning
In 2020-21, 44% of drug-related hospitalisations in Victoria were due to drug poisoning. Furthermore, 68% of drug poisoning related hospitalisations were intentional (75 hospitalisations per 100,000 people) and 19% were unintentional (20 hospitalisations per 100,000 people).
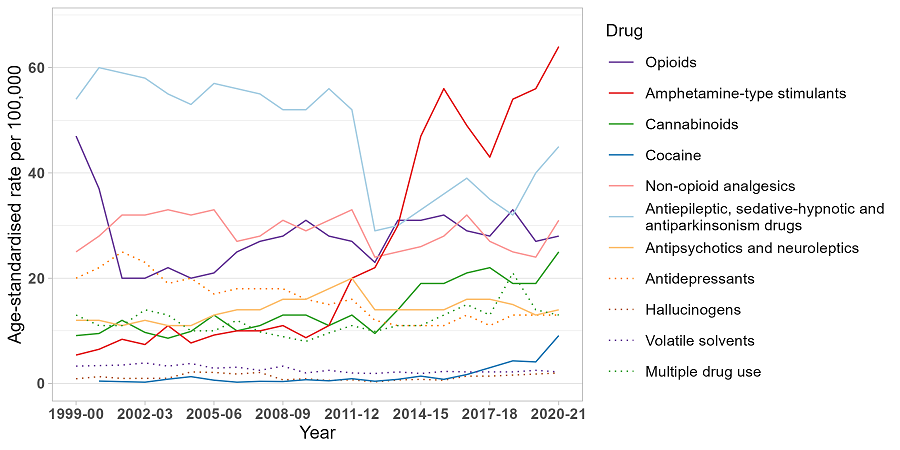
Drug Type
In 2020-21, the rate of hospitalisations was highest where there was a principal diagnosis indicating amphetamine-type stimulants (64 hospitalisations per 100,000 people).
Compared to 2019-20, there were significant increases in 2020-21 in the rates of hospitalisations related to: amphetamine-type stimulants; antiepileptic, sedative-hypnotic and antiparkinsonism drugs; non-opioid analgesics; opioids; cannabinoids; and cocaine (p<0.050).
Age-standardised rate per 100,000 people of drug-related hospitalisations, by sex, Victoria, 1999-00 to 2020-21.
Note: From 1st July 2011 to 30th June 2013 (i.e., between 2011-12 and 2012-13), there was a large decrease in public hospitalisations reported for the Victorian Admitted Episodes Dataset (VAED) because episodes where the patient’s entire care is provided in the emergency department were not considered for admission, irrespective of whether a criterion for admission is met. From 2013-14 onwards, “ED-only admissions” were largely replaced with admissions to Short Stay Observation Units.
Age-standardised rate per 100,000 people of drug-related hospitalisations, by remoteness, Victoria, 2012-13 to 2020-21.
Note: The size (area) of the bubble is proportional to the number of hospitalisations. The number of hospitalisations for remote and very remote Victoria in each year were small (less than or equal to 10) thus age-standardised rates were not calculated. Please refer to our methods document for details. Data on remoteness are only available from 2012-13.
Age-standardised rate per 100,000 people of drug-related hospitalisations, by principal diagnosis of mental and behavioural disorder due to substance use (A) and external cause of poisoning (B), Victoria, 1999-00 to 2020-21.
Age-standardised rate per 100,000 people of drug-related hospitalisations, by drug identified in the principal diagnosis, Victoria, 1999-00 to 2020-21.
Note: Age-standardised rates were not calculated if the number of hospitalisations was less than or equal to 10 (please refer to our methods document for details). Suppressed data are visible as gaps in the data series.
For complete report on trends in drug-related hospitalisations in Australia please go to the national report.
Acknowledgements
Funding
The Drug Trends program is funded by the Australian Government Department of Health and Aged Care under the Drug and Alcohol Program.
Data source
We would like to acknowledge the Australian Institute of Health and Welfare for data from the National Hospital Morbidity Database.
Acknowledgements
We would like to acknowledge the contribution of those who have been involved in past reporting on drug-related hospitalisations by Drug Trends, specifically: A/Prof Timothy Dobbins, Dr Amanda Roxburgh, and A/Prof Lucinda Burns.
We thank Dr Louise Tierney and her team from the Tobacco, Alcohol and Other Drugs Unit at the Australian Institute of Health and Welfare for reviewing the report.
We acknowledge the traditional custodians of the land on which the work for this report was undertaken. We pay our respects to Elders past, present, and emerging.
Related Links
- Hospitalisations data visualisations: https://drugtrends.shinyapps.io/hospital_separations
- Hospitalisations methods document: https://ndarc.med.unsw.edu.au/resource-analytics/trends-drug-related-hos...
- For other Drug Trends publications on drug-related hospitalisations and drug-induced deaths in Australia, go to: https://ndarc.med.unsw.edu.au/project/national-illicit-drug-indicators-p...
- For more information on NDARC research, go to: http://ndarc.med.unsw.edu.au/
- For more information about the AIHW and NHMD, go to: https://www.aihw.gov.au/
- For more information on ICD coding go to: http://www.who.int/classifications/icd/en/ https://www.ihacpa.gov.au/resources/icd-10-amachiacs-eleventh-edition
- For more research from the Drug Trends program go to: https://ndarc.med.unsw.edu.au/program/drug-trends
ISBN 978-0-7334-4058-8 ©NDARC, UNSW SYDNEY 2022
This report was prepared by researchers from the National Drug and Alcohol Research Centre for the Drug Trends program. The Drug Trends program is coordinated by the National Drug and Alcohol Research Centre, UNSW Sydney and undertaken in partnership with the Burnet Institute, National Drug Research Institute, University of Queensland, and University of Tasmania.
This work is copyright. You may download, display, print and reproduce this material in unaltered form only (retaining this notice) for your personal, non-commercial use or use within your organisation. All other rights are reserved. Requests and enquiries concerning reproduction and rights should be addressed to NDARC, UNSW Sydney, NSW 2052, Australia.
Recommended citation: Chrzanowska, A., Man, N., Akhurst, J., Sutherland, R., Degenhardt, L. & Peacock, A. (2022). Trends in drug-related hospitalisations in Australia, 1999-2021. Sydney: National Drug and Alcohol Research Centre, UNSW Sydney. DOI: 10.26190/wrsv-3b78
Please note that as with all statistical reports there is the potential for minor revisions to data in this report. Please refer to the online version at Drug Trends.
Please contact the Drug Trends team with any queries regarding this publication: drugtrends@unsw.edu.au.