This poster was presented by Elizabeth Whittaker at the 2015 NDARC Annual Research Symposium. The poster won the Judges Prize as well as the People's Choice Prize for "Outstanding research poster" at the Symposium.
Abstract
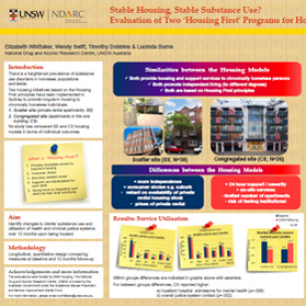
Background and aims: Australian and international evidence highlights the heightened prevalence of substance use disorders in homeless populations. In recent years, adaptations of the Housing First initiative, whereby chronically homeless individuals are provided long-term housing with support, have been implemented across Australia. Two such adaptions include scatter-site (private rental apartments; SS) and congregate site (apartments in the one building; CS) models. There is currently limited Australian evidence on the effect that these variations of Housing First programs have on client outcomes. The primary aim of this study is to undertake a longitudinal evaluation of two adaptations of the Housing First model (one SS and one CS) in relation to clients’ housing and health outcomes, specifically substance use patterns and service utilisation.
Methods: This paper draws upon the quantitative component of the longitudinal, mixed-methods design. Health and service utilisation outcome measures at baseline and 12 months post-baseline will be compared between SS and CS.
Results: A recruitment rate of 66% was achieved at baseline for both programs, of which 79% were successfully followed-up at 12 months post-baseline. Clients in both models did not differ significantly on demographics, homelessness history or proportion with a substance use disorder. However, at baseline a significantly higher proportion of clients in the CS model had an anxiety disorder (67% vs. 34%) and had recently injected (42% vs. 19%) than the SS model. Findings showed SS and CS participants had similar changes over time for use of specific substances and most health services. A greater increase in weekly injecting behaviour was found for CS participants, and criminal justice system contact decreased for SS but increased for CS.
Conclusions: While both models showed similar improvements in health outcomes, the variation between models observed for injecting behaviours and criminal justice system contact warrants further investigation to determine if the configuration of housing and support has a greater impact on the outcomes of particular individuals, such as people who inject drugs.
Implications of the research: While both programs house clients with complex needs, the analysis of client outcomes may hold important considerations for future housing policy decisions, as it will identify the health outcomes and government costs incurred by the housed individuals.